So, if gliadin is only partially digested when we eat it, and gliadin peptides are able to activate T cells, why doesn’t everyone who eats gluten develop celiac disease?
As described above, MHC class II proteins display peptides on the surface of antigen presenting cells for CD4+ T cells to recognize. There are 3 major types of MHC class II proteins: HLA-DP, HLA-DQ, and HLA-DR.
Of these 3 main MHC class II proteins, the HLA-DQ type is known to be involved in celiac disease.
All proteins have corresponding genes that provide the instructions to make them. The genes for MHC class II proteins are found on one of our chromosomes in a region known as the human leukocyte antigen (HLA) gene complex.
Each MHC class II protein is made up of two subunits (or parts), alpha and beta, that work together as a pair. The HLA-DQ protein is made of alpha and beta subunits encoded by the HLA-DQA1 and HLA-DQB1 genes.
The HLA-DQA1 and HLA-DQB1 genes are not the same in every person. These genes are polymorphic, which means they are variable from person to person and produce proteins that are slightly different from one another. These variations (called haplotypes) affect the way MHC class II proteins interact with the antigens they display and can determine whether or not CD4+ T cells recognize that antigen and begin an immune response. Certain MHC haplotypes cause some antigens (the “key”) to fight more snuggly within the T cell receptor (the “lock”). The better the fit, the stronger the immune response.
Most people with celiac disease have either the DQ2 or DQ8 haplotype.1 These haplotypes of MHC class II are able to present gliadin peptides to CD4+ T cells in a way that initiates an immune response.2
Why doesn’t everyone with HLA-DQ2 or HLA-DQ8 develop celiac disease?
Approximately 30% of the population (3 of every 10 people) has the DQ2 haplotype, yet only about 1% (1 of every 100) will develop celiac disease.1-3 Genetic testing for HLA-DQ2 or HLA-DQ8 can tell us who is predisposed (at risk) for developing celiac disease, but it currently can’t tell us who will develop the disease, or when it might be triggered.
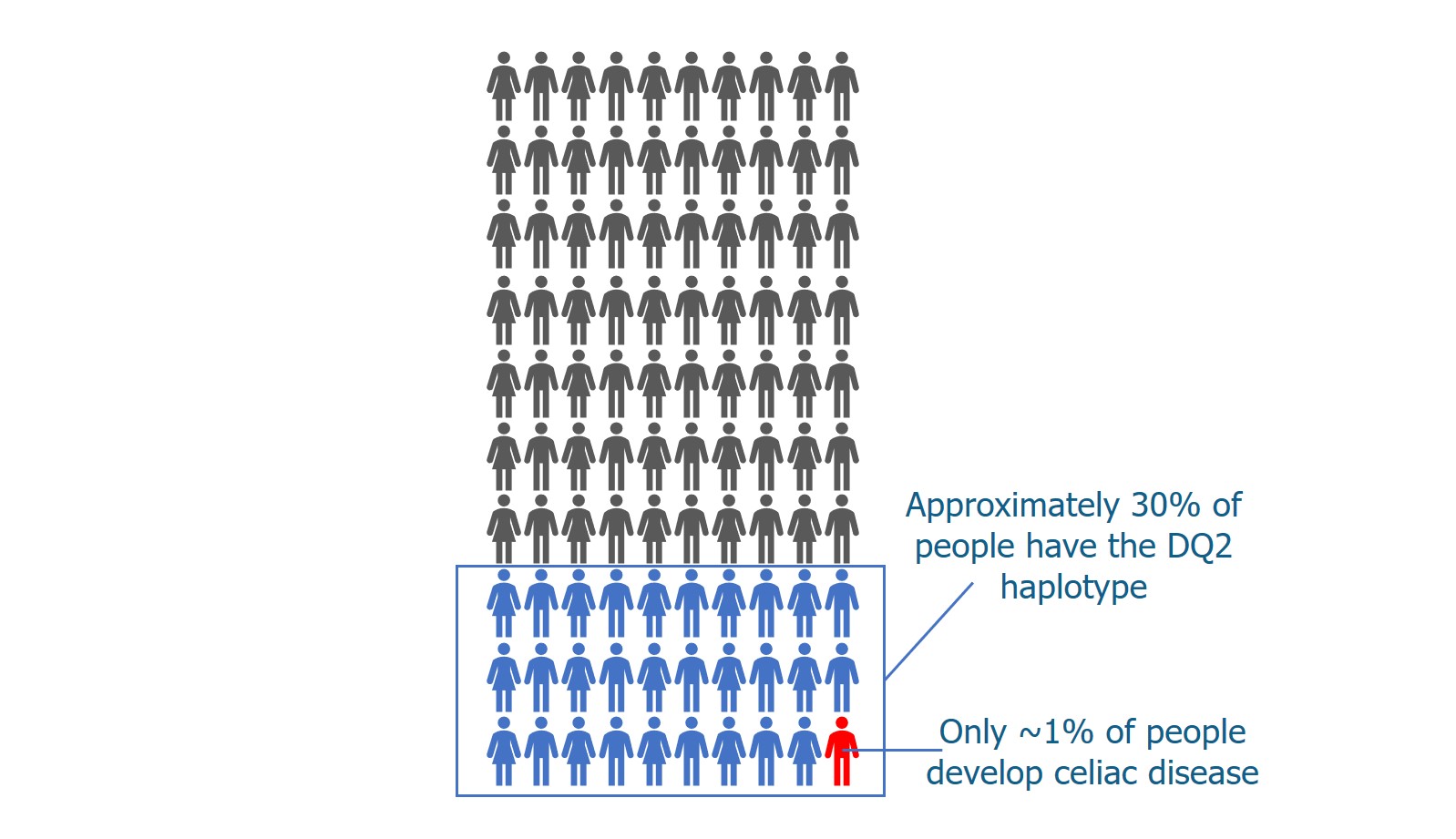
Researchers are trying to identify other factors that are involved in triggering celiac disease. They are studying whether things like other genes, our environment, bacteria that normally live in our gut (our microbiome), or previous infections may play a role.
NEXT TOPIC: What role does tissue transglutaminase play in celiac disease?
REFERENCES
- Gujral N, Freeman HJ, Thomson AB. Celiac disease: prevalence, diagnosis, pathogenesis and treatment. World J Gastroenterol. 2012;18(42):6036-6059.
- Singh P, Arora A, Strand TA, et al. Global Prevalence of Celiac Disease: Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2018.
- Fasano A, Berti I, Gerarduzzi T, et al. Prevalence of celiac disease in at-risk and not-at-risk groups in the United States: a large multicenter study. Arch Intern Med. 2003;163(3):286-292.
GLOSSARY
Antigen – A protein that is recognized by an immune cell receptor and triggers an immune response.
Antigen presenting cell – A specialized immune cell that presents peptides to CD4+ or CD8+ T cells. Peptides are presented by MHC I or MHC II proteins.
Gliadin – One of the wheat proteins that forms gluten. Responsible for triggering an immune response in patients with celiac disease.
Gluten – A type of protein found in cereal grains. Wheat gluten is made of two proteins called gliadin and glutenin.
Haplotype – Variations in HLA genes that produce different MHC class II proteins.
HLA gene complex – Human leukocyte antigen (HLA) gene complex is a region on our chromosomes that contains the genes that produce MHC class II proteins.
HLA-DQ – The HLA haplotype that is associated with celiac disease.
MHC class II protein – Major histocompatibility complex class II protein. Found on the surface of antigen presenting cells. Presents peptides to CD4+ T cells.
Peptide – A small protein fragment consisting of a chain of amino acids.
Polymorphic – Variable from person to person.
Receptor – A protein that is located on the surface of a cell and interacts with other proteins. Receptors act as the “locks” that recognize specific pathogen “keys”.
T cell – A type of adaptive immune cell. Also called T lymphocyte.
Share this Post
